Abstract
Objectives: The study aims were to measure the prevalence of hypochondriasis among medical students, King Saud University (KSU). Methodology: Cross-sectional study targeted 400 KSU medical students divided into eight subgroups according to their gender and academic level. 350 of whom responded (87.5%). The questioner was designed by the research team based on DSM - IV criteria to cover most aspect s of presentations of hypochondriasis. Only students who were diagnosed of having hypochondriasis by a medical doctor at time of the study were included in the prevalence measurement. Results: The overall prevalence of hypochondriasis among KSU medical students was 3.4%. The prevalence among male students was 2.9% while it was 3.8% among female students (p=0.678). The prevalence among basic -year students was 3.1% compared to 3.8% among clinical-year students (p=0.734). Conclusions and recommendations: The overall prevalence of hypochondriasis among medical students was 3.4%, but there was no significant difference based on gender or academic level of the students. We recommend further studies with larger sample size that include different medical colleges from different regions of Saudi Arabia.
Keywords: Hypochondriasis, prevalence, medical students
Introduction
Hypochondriasis is a medical condition and a part of somatoform disorders. Somatoform disorders are a group of psychiatric illnesses characterized by having physical symptoms that has no identifiable cause, and patients believe that a disease or more causes these symptoms. Hypochondriasis is a condition characterized by a prolonged, strong fear of a serious disease or a conviction that they already have it, while they don’t. Medical evaluation and reassurance of their good health doesn’t relieve or convince patients that they don’t have the disease. They usually misinterpret their sensations or minor symptoms to fit with their feared illness. Hypochondriasis is diagnosed using the Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria. The DSM-IV diagnostic criteria for hypochondriasis includes: Preoccupation with fears that the patient has, or will have, a serious illness based on their misinterpretation of symptoms, that fear is not relieved by appropriate medical reassurance, and that lasts for at least 6 months (American Psychiatric Association, 2000)
Our literature review about studies concerning hypochondriasis revealed an increase in prevalence of hypochondriasis among medical students compared to other university students. It was also revealed that first year medical students are more prevalent to hypochondriasis than third year medical students (Moss-Morris & Petrie, 2001). Other studies showed no significant difference between third and fourth year medical students in the prevalence of hypochondriasis. That study also showed that 30% of medical students reported a history of hypochondriasis, and only 22% of them consulted a medical specialist. It was also found that age and gender has no significant association with the diagnosis of hypochondriasis (Candel, 2003).
The prevalence of hypochondriasis in the general population of Germany based on the item questions of DSM-IV was found to be low (0.05%), while it was higher (0.58%) using less restrictive diagnostic criteria than DSM-IV (Martin & Jacobi, 2006). In a study conducted in Australia to measure the prevalence of somatization among Australian general practice attendees revealed that 18.6% of patients were somatisers, and there was an increase in the prevalence of depression and anxiety among them (Clarke, Piterman, Byrne, & Austin, 2008).
Up to our searching effort and knowledge, there was no published study about the prevalence of hypochondriasis among medical students in Saudi Arabia. That supported us to look for this particular aspect of research. This study aims was to measure the prevalence of hypochondriasis among medical students, compare the results based on gender and academic level of medical students.
Material and Method
A cross-sectional study was performed. The target population was King Saud University medical students of both genders and on different academic levels. The sample size was 400 students divided into eight subgroups among the academic years 1st to 4th. 2 subgroups, one for males and the other for females with a ratio of 1:1 covered each academic year. 350 of whom responded (87.5%).
The questionnaire was designed by the research team based on DSM-IV to cover most aspects of hypochondriasis among medical students, compare the results based on gender and academic level of students. Basic years were defined to be 1st and 2nd, while Clinical practice years were defined as 3rd and 4th. The questionnaires, therefore, included the following variables, demographic data that were gender, age, place of residence and academic year. The hypochondriasis-related variables in the questionnaire included –but not only-fear of disease, feeling symptoms, difficulty in trusting doctors' reassurance, that these previous items persisted for the past 6 months, and an inquiry if they were currently medically diagnosed of having hypochondriasis.
Our prevalence measurement was mainly based on students who were diagnosed of having hypochondriasis by a medical doctor at the time of data collection.
The questionnaires were distributed to the respondents through students’ class leaders, independent from the research team influence, and the leaders were totally unaware of the objectives of the research.
The data collection was carried out from 18/2/2010 to 25/2/2010. The response rate was 87.5%. All collected questionnaires were counted and included in the analysis that was done using Statistical Package for Social Sciences (SPSS) program, version 11. Chi-square was calculated to define the significance and directions of association between the study variables. P value was considered to be significant if it was less than 0.05%
Results
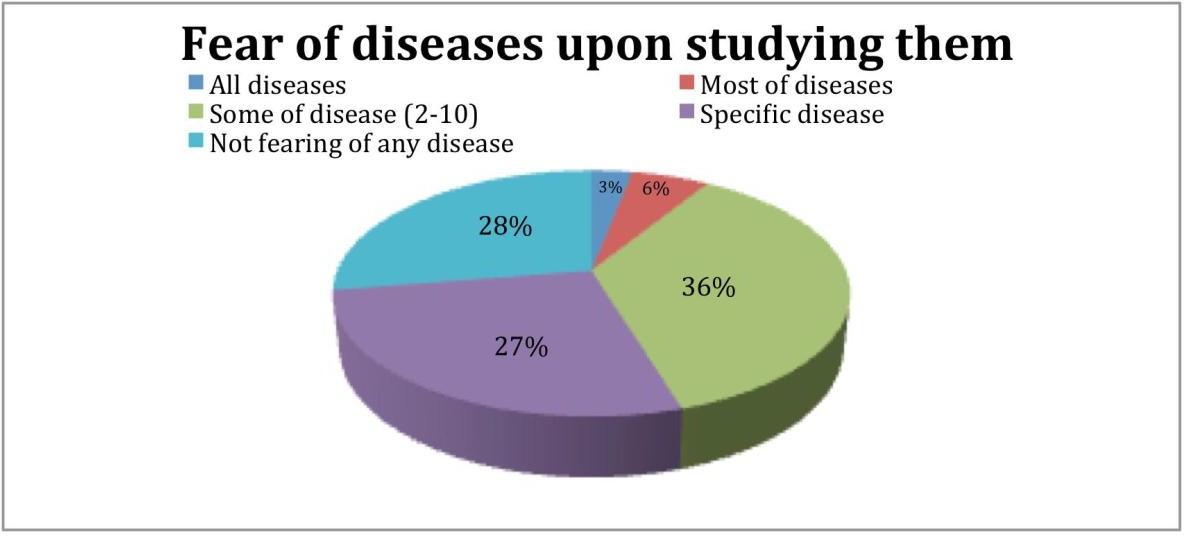
The study showed that the overall prevalence of hypochondriasis among KSU medical students was 3.4%. The prevalence among male students was 2.9% and was 3.8% among female students (p=0.678). The prevalence among basic-year students was 3.1% while it was 3.8% among clinical-year students (p=0.734). Further detail of study is in tables 1-8 and figure 1. 4.3% of the students met the following DSM-IV criteria for hypochondriasis: excessive worry of getting a serious disease, felt symptoms and though it may indicate a serious disease, had a difficulty in believing doctor’s reassurance, and those previous items persisted for the prior 6 months of data collection. 40% of them were males, while 60% were females (p=0.5). 66.7% of students who met the mentioned criteria were basic-year students, while 33.3% of them were clinical-year students (p=0.8). The percentage of students who feared getting a serious illness was 33%.
Discussion and Conclusion
Hypochondriasis is a medical psychiatric condition under the group of somatoform disorders. Patients with this disorder are convinced that they have a serious disease or very worried of getting one based on their misinterpretation of symptoms for at least 6 months. In a study conducted at Mashhad University of Medical Sciences, the prevalence of hypochondriasis among medical students was found to be 16%, and there was a highly significant increase in the prevalence among female medical students compared to males (p=0.000) (Talaei, 2002). The prevalence of hypochondriasis in general population based on DSM-IV was suggested to be unknown in a previous study, others mentioned that its prevalence among primary care patients was in the range between 0.8 to 4.5% (Magarinos, Zafar, Nissenson, & Blanco, 2002). The point prevalence of hypochondriasis among German population using DSM-IV criteria revealed in a study that 0.4% of population fulfilled the criteria for hypochondriasis, it was also suggested that the prevalence was more in female gender, higher age, and lower school education. This study also suggested using a less restrictive diagnostic criteria than DSM-IV (Bleichhardt & Hiller, 2007) Other study also supported that there was an increase in prevalence of hypochondriasis in those with low years of education, but didn’t find a predominance among females (Creed & Barsky, 2004).
In another study, the research team designed new criteria other than DSM-IV to diagnose hypochondriasis and compared the prevalence of hypochondriasis based on their new criteria with those of DSM-IV. They classified patients diagnosed with hypochondriasis into mild and severe cases. The prevalence of severe cases among primary care patients based on their new criteria was 9.5%, while it was 5.9% based on DSM-IV. It was also mentioned that their new criteria has less overlap with other somatoform disorders than DSM-IV. However, the new criteria was said to be preliminary and need to be supported (Fink, Ornbol, Toft, Sparle, Frostholm, & Olesen, 2004). Ruling out panic disorder before diagnosing patients with hypochondriasis was recommended in a study if patients have any symptoms of panic disorders that can be similar to the fear and worry hypochondriacs have (Scrignar, 2004).
Regarding the association between hypochondriasis and personality disorders, a study showed a high prevalence of personality disorders among patients with hypochondriasis. The most common associated type of personality disorder with hypochondriasis was obsessive-compulsive personality disorder (Sakai, Nestoriuc, Nolido, & Barsky, 2010).
In a randomized controlled study, Psychotherapy have shown a reduction in symptoms in patients with hypochondriasis compared to control groups in the short term (Bouman, 2008). Cognitive behavioral therapy and paroxetine were both found to be effective treatments of hypochondriasis for the long term (Greeven et al., 2009). In another review article, it was revealed that chronic pain was associated with hypochondriasis and that treating pain would improve patients with hypochondriasis (Fishbain, Lewis, Gao, Cole, & Steele Rosomoff, 2009). Regarding the assessment of prognostic factors of hypochondriasis, a review article showed that 30% to 50% of patients would recover (Hartman et al, 2009).
Some studies suggested that hypochondriasis is more of an anxiety disorder than a somatoform disorder (Abramowitz, Schwartz, & Whiteside, 2002; Olatunji, Deacon, & Abramowitz, 2009). While others suggested that it’s an interim between them but closer of being among anxiety disorders (Gropalis, Bleichhardt, Witthoft, & Hiller, 2012). Hypochondriasis was classified in a study into two dimensions: disease phobia and disease conviction (Fergus & Valentiner, 2010).
Compared to our literature review, the prevalence of hypochondriasis among medical students at KSU was lower than most papers (Candel, 2003; Talaei, 2002).
Unlike a previous study that showed an increase in prevalence of hypochondriasis among first year medical students compared to third year students (Moss-Morris & Petrie, 2001), we didn’t find any significant difference based on academic level of medical students in the prevalence of hypochondriasis. Our results were also supported by previous studies that suggested no difference in the prevalence based on age or gender of the students (Candel, 2003).
Supported by previous studies (Creed & Barsky, 2004), we didn’t find any significant difference based on gender in the prevalence of hypochondriasis among medical students. While other studies suggested a highly significant increase in prevalence among female medical students (p=0.000) (Talaei, 2002), and another one which found an increase in the prevalence among females in the general population of Germany (Magarinos et al., 2002).
However, we have found that there was a significant difference based on gender regarding the item of increase in severity of symptoms after reading about it. 37.5% of female medical students from different academic levels showed that, compared to 28.8% of male medical students (p=0.05).
We also have found that there was significant difference based on the academic level in students who tried to treat their symptoms based on their medical knowledge without medical consultation. 40.9% of students in the clinical years tried to do so, while 29.8% of students in basic years did, (p=0.03).
In Conclusion: the overall prevalence of hypochondriasis was 3.4%, and there was no significant difference based on gender or academic level of the students.
The Limitation of this study was due to that the sample size was small in number and it was only in one medical college. We recommend further studies with larger sample size that include different medical colleges from different regions of Saudi Arabia.
Acknowledgements
We would like to thank all the persons who helped us through this study. Those persons who gave effort for us to collect samples, analyze it, and write the paper.
We would like to thank Dr. Aws S. Almufleh for his great effort to help us analyze our data us ing SPSS. We also would like to thank the male group leaders: Ahmed Almazrou, Mohammed AlKhuraiji, and Mohammed AlKhamees for their effort to distribute the samples to the students of their years. We are also so grateful to Rowayda Mishiddi, and to Marwa Hassona for their effort to distribute the samples for female students.
The author(s) declare that there is no conflict of interest.
References
American Psychiatric Association. (2000). Diagnostic and Statistical M anual of Mental Disorders, 4th Edition, Text Revision (DSM - IV-TR): American Psychiatric Association.
Moss-Morris, R., & Petrie, K. J. (2001). Redefining medical students' disease to reduce morbidity. Medical education, 35(8), 724-8.
Candel, I. (2003). Fantasy proneness and thought suppression as predictors of the Medical Student Syndrome. Personality and individual differences, 35, 519 -24.
Martin, A., & Jacobi F. (2006). Features of hypochondriasis and illness worry in the general population in Germany. Psychosomatic medicine, 68(5), 770-7.
Clarke, D. M., Piterman, L., Byrne, C. J., & Austin, D. W. (2008). Somatic symptoms, hypochondriasis and psychological distress: a study of somatisation in Australian general practice. The Medical journal of Australia, 189(10), 560-564.
Talaei A. (2009). Hypochondriasis in medical sciences students of Mashhad, Iran. European Psychiatry, 24.
Magarinos, M., Zafar, U., Nissenson, K., & Blanco, C. (2002). Epidemiology and treatment of hypochondriasis. CNS drugs, 16(1), 9-22.
Bleichhardt, G., & Hiller, W. (2007). Hypochondriasis and health anxiety in the German population. British journal of health psychology, 12(4), 511-23.
Creed, F., & Barsky, A. A. (2004). systematic review of the epidemiology of somatisation disorder and hypochondriasis. Journal of psychosomatic research, 56(4), 391-408.
Fink, P., Ornbol, E., Toft, T., Sparle, K. C., Frostholm, L., & Olesen, F. (2004). A new, empirically established hypochondriasis diagnosis. The American journal of psychiatry, 161(9), 1680-1691.
Scrignar, C. B. (2004). Hypochondriasis or panic disorder? The Journal of the Louisiana State Medical Society: official organ of the Louisiana State Medical Society, 156(4), 200-2.
Sakai, R., Nestoriuc, Y., Nolido, N. V., & Barsky, A. J. (2010). The prevalence of personality disorders in hypochondriasis. The Journal of clinical psychiatry, 71(1), 41 -7.
Bouman, T. K. (2008). Review: psychotherapy may be beneficial for people with hypochondriasis. Evidence-based mental health, 11(3), 90.
Greeven, A., van Balkom, A. J., van der Leeden, R., Merkelbach, J. W., van den Heuvel, O. A., & Spinhoven, P. (2009). Cognitive behavioral therapy versus paroxetine in the treatment of hypochondriasis: an 18 -month naturalistic follow-up. Journal of behavior therapy and experimental psychiatry. 40(3), 487-496.
Fishbain, D. A., Lewis, J. E., Gao, J., Cole, B., & Steele Rosomoff, R. (2009). Is chronic pain associated with somatization/hypochondriasis? An evidence -based structured review. Pain practice: the official journal of World Institute of Pain, 9(6), 449-67.
Hartman, T. C., Borghuis, M. S., Lucassen, P. L., van de Laar, F. A., Speckens, A. E., & van Weel, C. (2009). Medically unexplained symptoms, somatisation disorder and hypochondriasis: course and prognosis. A systematic review. Journal of psychosomatic research, 66(5), 363-77.
Abramowitz, J. S., Schwartz, S. A., & Whiteside, S. P. (2002). A contemporary conceptual model of hypochondriasis. Mayo Clinic proceedings Mayo Clinic, 77(12), 1323-30.
Olatunji, B. O., Deacon, B. J., & Abramowitz, J. S. (2009). Is hypochondriasis an anxiety disorder? The British Journal of Psychiatry, 194(6), 481-2.
Gropalis, M., Bleichhardt, G., Witthoft, M., & Hiller, W. (2012). Hypochondriasis, somatoform disorders, and anxiety disorders: sociodemographic variables, general psychopathology, and naturalistic treatment effects. The Journal of nervous and mental disease, 200(5), 406-12.
Fergus, T. A., & Valentiner, D. P. Disease phobia and disease conviction are separate dimensions underlying hypochondriasis. Journal of behavior therapy and experimental psychiatry, 41(4), 438-444.
Copyright information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.